Some children with autism experience profound, lifelong difficulties like developmental delay, social struggles and even the inability to speak. Others experience more mild symptoms that improve with time.
The disparity in outcomes has been a mystery to scientists, until now. A new study, published in Molecular Autism by researchers at University of California San Diego, is the first to shed light on the matter. Among its findings: The biological basis for these two subtypes of autism develops in utero.
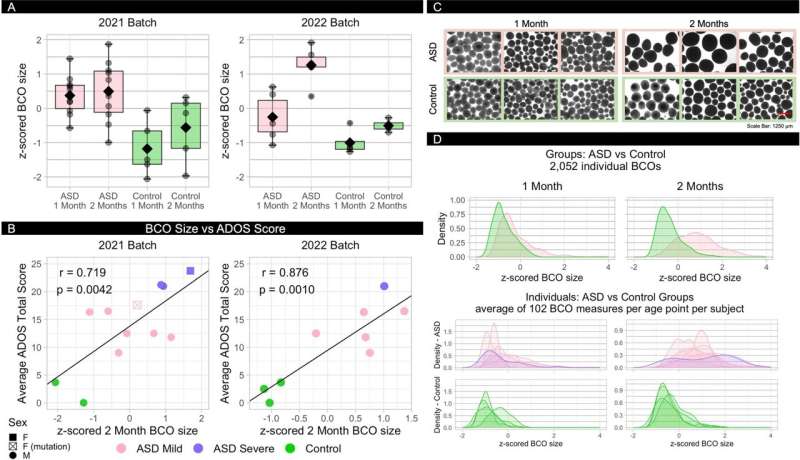
Researchers used blood-based stem cells from 10 toddlers, ages 1 through 4, with idiopathic autism (in which no single-gene cause was identified) to create brain cortical organoids (BCOs), or models of the fetal cortex. They also created BCOs from six neurotypical toddlers.
Often referred to as gray matter, the cortex lines the outside of the brain. It holds tens of billions of nerve cells and is responsible for essential functions like consciousness, thinking, reasoning, learning, memory, emotions and sensory functions.
Among their findings: The BCOs of toddlers with autism were significantly larger—roughly 40 percent—than those of neurotypical controls, according to two rounds of study performed in different years (2021 and 2022). Each round involved the creation of hundreds of organoids from each patient.

The researchers also found that abnormal BCO growth in toddlers with autism correlated with their disease presentation. The larger a toddler’s BCO size, the more severe their social and language symptoms were later in life, and the larger their brain structure on MRI. Toddlers with excessively enlarged BCOs showed greater-than-typical volume in social, language and sensory brain areas when compared to neurotypical peers.
“The bigger the brain, the better isn’t necessarily true,” said Alysson Muotri, Ph.D., director of the Sanford Stem Cell Institute (SSCI) Integrated Space Stem Cell Orbital Research Center at the university. The SSCI is directed by Catriona Jamieson, M.D., Ph.D., a leading physician-scientist in cancer stem cell biology whose research explores the fundamental question of how space alters cancer progression.
“We found that in the brain organoids from toddlers with profound autism, there are more cells and sometimes more neurons—and that’s not always for the best,” added Muotri, who is also a professor in the Departments of Pediatrics and Cellular and Molecular Medicine at the UC San Diego School of Medicine.
What’s more, the BCOs of all children with autism, regardless of severity, grew roughly three times faster than those of neurotypical children. Some of the largest brain organoids—from children with the most severe, persistent cases of autism—also saw the accelerated formation of neurons. The more severe a toddler’s autism, the quicker their BCO grew—sometimes to the point of developing an excess of neurons.
Eric Courchesne, Ph.D., a professor in the School of Medicine’s Department of Neurosciences who co-led the research with Muotri, called the study “one of a kind.” Matching data on children with autism—including their IQs, symptom severity and imaging like MRIs—with their corresponding BCOs or similar stem cell-derived models makes an incredible amount of sense, he said. But oddly enough, such research hadn’t been undertaken ahead of their work.
“The core symptoms of autism are social affective and communication problems,” said Courchesne, who also serves as co-director of the UC San Diego Autism Center of Excellence. “We need to understand the underlying neurobiological causes of those challenges and when they begin. We are the first to design an autism stem cell study of this specific and central question.”
It’s long been assumed that autism, a complex pool of progressive disorders, begins prenatally and involves multiple stages and processes. While no two people with autism are like—just as no two neurotypical people are—those with the neurodevelopmental condition can generally be grouped into two categories: those who have severe social struggles and require lifelong care, and may even be nonverbal, and those who have a milder version of the condition who eventually develop good language skills and social relationships.
Scientists haven’t been able to ascertain why at least two groups of individuals with autism exist. They also haven’t been able to prenatally identify children with autism, let alone predict how severe their condition might be.
Now that Courchesne and Muotri have established that brain overgrowth begins in the womb, they hope to pinpoint its cause, in a bid to develop a therapy that might ease intellectual and social functioning for those with the condition.
Co-authors of the study include Vani Taluja, Sanaz Nazari, Caitlin M. Aamodt, Karen Pierce, Kuaikuai Duan, Sunny Stophaeros, Linda Lopez, Cynthia Carter Barnes, Jaden Troxel, Kathleen Campbell, Tianyun Wang, Kendra Hoekzema, Evan E. Eichler, Joao V. Nani, Wirla Pontes, Sandra Sanchez Sanchez, Michael V. Lombardo and Janaina S. de Souza.
More information:
Eric Courchesne et al, Embryonic origin of two ASD subtypes of social symptom severity: the larger the brain cortical organoid size, the more severe the social symptoms, Molecular Autism (2024). DOI: 10.1186/s13229-024-00602-8
Citation:
Brain overgrowth dictates autism severity, new research suggests (2024, June 5)
retrieved 5 June 2024
from https://medicalxpress.com/news/2024-06-brain-overgrowth-dictates-autism-severity.html
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no
part may be reproduced without the written permission. The content is provided for information purposes only.

